Should every day be Meatless Monday?
Posted Jan 19, 2019

Source: Suzi Smith / used with permission
An important new study about global nutrition was published this week that deserves everyone’s full attention: "Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems." [Don’t let the title intimidate you: You need to know what’s inside.] This paper was commissioned and published by The Lancet — one of the world’s oldest and most respected medical journals — and penned by an international group of 37 scientists led by Dr. Walter Willett of Harvard University.
The product of three years of deliberation, this 47-page document envisions a “Great Food Transformation” which seeks to achieve an environmentally sustainable and optimally healthy diet for the world’s people by 2050. Its core recommendation is to minimize consumption of animal foods as much as possible, and replace them with whole grains, legumes, and nuts.
Source: EAT-Lancet Commission report
We all want to be healthy, and we need a sustainable way to feed ourselves without destroying our environment. The well-being of our planet and its people are clearly in jeopardy, therefore clear, science-based, responsible guidance about how we should move forward together is most welcome.
Unfortunately, we are going to have to look elsewhere for solutions, because the report fails to provide us with the clarity, transparency and responsible representation of the facts we need to place our trust in its authors. Instead, the Commission’s arguments are vague, inconsistent, unscientific, and downplay the serious risks to life and health posed by vegan diets.
1. Nutrition epidemiology = mythology
The vast majority of human nutrition research — including the lion share of the research cited in the EAT-Lancet report — is conducted using the tragically flawed methodology of nutrition epidemiology. Nutrition epidemiology studies are not scientific experiments; they are wildly inaccurate, questionnaire-based guesses (hypotheses) about the possible connections between foods and diseases. This approach has been widely criticized as scientifically invalid [see here and here], yet continues to be used by influential researchers at prestigious institutions, most notably Dr. Walter Willett. An epidemiologist himself, he wrote an authoritative textbook on the subject and has conducted countless such studies, including a recent, widely-publicized paper tying low-carbohydrate diets to early death. In my reaction to that study, I explain in plain English why epidemiological techniques are so untrustworthy and include a sample from an actual food questionnaire for your amusement.
Even if you think epidemiological methods are sound, at best they can only generate hypotheses that then need to be tested in clinical trials. Instead, these hypotheses are often prematurely trumpeted to the public as implicit fact in the form of media headlines, dietary guidelines, and well-placed commission reports like this one. Tragically, more than 80% of these guesses are later proved wrong in clinical trials. With a failure rate this high, nutrition epidemiologists would be better off flipping a coin to decide which foods cause human disease. The Commission relies heavily on this methodology, which helps to explain why its recommendations often fly in the face of biological reality.
2. Red meat causes heart disease, diabetes, cancer... and spontaneous combustion
The section of the report dedicated to protein blames red meat for heart disease, stroke, type 2 diabetes, obesity, cancer, and early death. It contains 16 references, and every single one is an epidemiological study. The World Health Organization report tying red meat to colon cancer was also mentioned, and that report is almost entirely based on epidemiology as well. [Read my full analysis of the WHO report here.] The truth is that there is no human clinical trial evidence tying red meat to any health problem. I certainly haven’t found any — and if there were, I think this Commission surely would have mentioned it.
Yet even in this “red meat is an apocalypse on a plate” section, meat’s virtues peek through:
[In sub-Saharan Africa] “...growing children often do not obtain adequate quantities of nutrients from plant source foods alone…promotion of animal source foods for children, including livestock products, can improve dietary quality, micronutrient intake, nutrient status, and overall health.”
3. Protein is essential… but cancerous
The commissioners write:
“Protein quality (defined by effect on growth rate) reflects the amino acid composition of the food source, and animal sources of protein are of higher quality than most plant sources. High-quality protein is particularly important for growth of infants and young children, and possibly in older people losing muscle mass in later life.”
Translation: Complete proteins are good because they contain every essential amino acid. All animal proteins are naturally complete, whereas most plant proteins are incomplete. Watch how the authors wriggle their way out of this inconvenient truth in the next sentence:
“However, a mix of amino acids that maximally stimulate cell replication and growth might not be optimal throughout most of adult life because rapid cell replication can increase cancer risk.”
Translation: Complete proteins are bad because they cause cancer.
The sole reference for this absurd suggestion that complete proteins cause cancer is a paper about mutations causing cancer in which the terms “protein,” “amino acid,” and “meat” each occur a grand total of zero times, suggesting that the Commission’s suggestion is pure... suggestion. Furthermore, if obtaining all of the essential amino acids we need causes cancer, shouldn't we also worry about complete proteins from plant sources like tofu or beans with rice?
4. Omega-3s are essential... good luck with that
“Fish has a high content of omega-3 fatty acids, which have many essential roles… Plant sources of alpha-linolenic acid [ALA] can provide an alternative to omega-3 fatty acids, but the quantity required is not clear.” [page 11]
If the Commission doesn’t know how much plant ALA a person needs to consume to meet requirements, then how does it know that plants provide a viable alternative to omega-3s from animal sources?
The elephant in the room here is that all omega-3s are not created equal. Only animal foods (and algae, which is neither a plant nor an animal) contain the forms of omega-3s our bodies use: EPA and DHA. Plants only contain ALA, which is extremely difficult for our cells to convert into EPA and DHA. According to this 2018 review, we transform anywhere between 0% and 9% of the ALA we consume into the DHA our cells require.
Instead of being vague, why not responsibly warn people that trying to obtain omega-3 fatty acids from plants alone may place their health at risk?
“About 28 g/day (1 ounce) of fish can provide essential omega-3 fatty acids… therefore we have used this intake for the reference diet. We also suggest a range of 0 – 100 g/day because high intakes are associated with excellent health.”
Wait… if it takes 28 grams to meet your daily requirement for omega-3s AND high intakes are associated with excellent health, why allow the range to begin at ZERO grams per day? If the Commission doesn’t feel comfortable recommending fish, it should at least recommend algae-sourced omega-3 supplements.
5. Vitamins and minerals are essential… so take supplements
The drumbeat heard throughout the report is that animal foods are dangerous and that a vegan diet is the holy grail of health, yet EAT-Lancet commissioners repeatedly find themselves in the awkward position of having to acknowledge the nutritional superiority of the very animal foods they recommend avoiding:
"Although inclusion of some animal source foods in maternal diets is widely considered important for optimal fetal growth and increased iron requirement, especially during the third trimester of pregnancy, evidence suggests that balanced vegetarian diets can support healthy fetal development, with the caveat that strict vegan diets require supplements of vitamin B12."
“Adolescent girls are at risk of iron deficiency because of rapid growth combined with menstrual losses. Menstrual losses have sometimes been a rationale for increased consumption of red meat, but multivitamin or multimineral preparation provide an alternative that is less expensive and without the adverse consequences of high red meat intake.” [page 13]
If the commissioners are concerned that red meat is dangerous (which is only true on Planet Epidemiology), why not recommend other naturally iron-rich animal foods such as duck, oysters, or chicken liver for these growing young women, as these foods would also provide the complete proteins needed for growth? What about the 10-22% of non-teen reproductive-age women in the U.S. who suffer from iron deficiency? And why a “multimineral preparation” rather than a simple iron supplement? Are they implying that other minerals may be lacking in their plant-based diet?
In changing to the EAT-Lancet diet, the Commission claims:
“The adequacy of most micronutrients increases, including several essential ones, such as iron, zinc, folate, and vitamin A, as well as calcium intake in low-income countries. The only exception is vitamin B12 that is low in animal-based diets [I believe this was an error on their part, since B12 is only found in animal foods.] Supplementation or fortification with vitamin B12 (and possibly with riboflavin [vitamin B2]) might be necessary in some circumstances.”
Unfortunately, the nutritional inadequacy of plant-based diets goes beyond B vitamins. Plant foods lack several key nutrients, and some of the nutrients they do contain come in less bioavailable forms. Furthermore, many plant foods contain “anti-nutrients” that interfere with nutrient absorption. This means that just because a plant food contains a nutrient doesn’t mean we can access it.
An important example is that grains, beans, nuts, and seeds — the staple foods of plant-based diets — contain phytate, a mineral magnet which substantially interferes with absorption of essential minerals like zinc, calcium, iron, and magnesium. And thanks to oxalates — mineral-binding compounds found in a wide variety of plant foods — virtually none of the iron in spinach makes it into Popeye’s muscles.
Only animal foods contain every nutrient we need in its proper, most accessible form. To learn more about nutrient availability and how it affects brain health, read this article.
6. Making up numbers is fun and easy
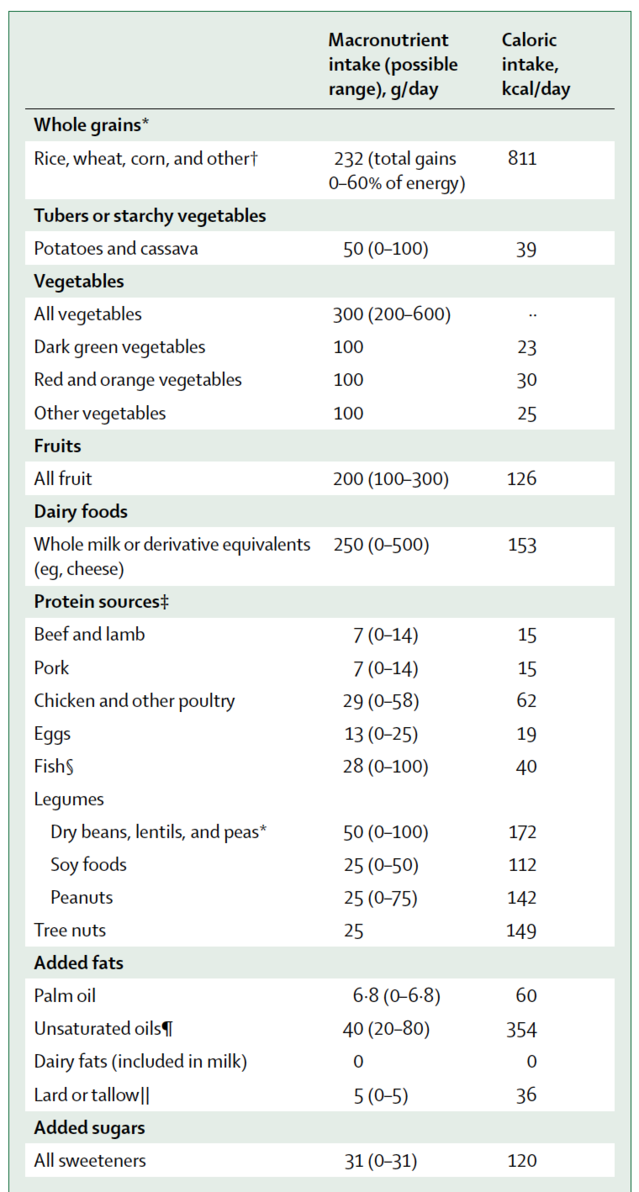
How did the commissioners arrive at the recommended quantities of foods we should eat per day… 7 grams of this, 31 grams of that? Numbers like these imply that something’s been precisely measured, but in many cases, it’s plain that they simply pulled a number out of thin air:
“Since consumption of poultry has been associated with better health outcomes than has red meat, we have concluded that the optimum consumption of poultry is 0 g/day to about 58 g/day and have used a midpoint of 29 g/day for the reference.”
Nowhere do they say that poultry is associated with any negative health outcomes, so why limit it to a maximum of 58 grams (2 ounces) per day?
The commissioners attempt to defend themselves from criticism on this issue by stating:
“We have a high level of scientific certainty about the overall direction and magnitude of associations described in this Commission, although considerable uncertainty exists around detailed quantifications.”
If they are this uncertain about the details, how can they in good conscienceprescribe such specific quantities of food? Why not say they don’t know? Most people will not read this report — they will interpret the values in this table as medical advice.
7. Epidemiology is gospel… unless we don’t like the results
Any researcher will tell you that clinical trials — actual scientific experiments — are considered a much higher level of evidence than epidemiological studies, yet Willett’s group not only relies heavily on epidemiological studies, it favors them over clinical trials when it suits their agenda:
“in large prospective [epidemiological] studies, high consumption of eggs, up to one a day, has not been associated with increased risk of heart disease, except in people with diabetes.
“However, in low-income countries, replacing calories from a staple starchy food with an egg can substantially improve the nutritional quality of a child’s diet and reduce stunting. [randomized clinical trial]“We have used an intake of eggs at about 13 g/day, or about 1.5 eggs per week, for the reference diet, but higher intake might be beneficial for low-income populations with poor dietary quality.” [page 11]
Why recommend only 1.5 eggs per week when epidemiological studies found that 1 egg per day was perfectly fine? And why skew your recommendations against low-income people, who make up a significant portion of the global population?
There is a remarkable paragraph on page 9 (too long to quote here) arguing that red meat was found to increase the risk of death in epidemiological studies conducted in Europe and the USA, but not in Asia, where red meat (mainly pork) was associated with a decreased risk of death. Rather than grappling with this seeming contradiction, the Commission simply dismisses the Asian findings as invalid, wondering if perhaps Asian countries haven’t been rich long enough for the risk to show up yet.
Wait. What?
8. Everyone should eat a vegan diet, except for most people
Although their diet plan is intended for all “generally healthy individuals aged two years and older,” the authors admit it falls short of providing proper nutrition for growing children, adolescent girls, pregnant women, aging adults, the malnourished, and the impoverished — and that even those not within these special categories will need to take supplements to meet their basic requirements.
Sadder still is the fact that the majority of people in this country and in many other countries around the world are no longer metabolically healthy, and this high-carbohydrate plan doesn’t take them into consideration.
"In controlled feeding studies, high carbohydrate intake increases blood triglyceride concentrations, reduces HDL [aka “good”] cholesterol concentration, and increases blood pressure, especially in people with insulin resistance.”
For those of us with insulin resistance (aka “pre-diabetes”) whose insulin levels tend to run too high, the Commission’s high-carbohydrate diet — based on up to 60% of calories from whole grains, in addition to fruits and starchy vegetables — is potentially dangerous. The Commission half-acknowledges this by recommending that even healthy people limit consumption of starchy roots like potatoes and cassava flour due to their high glycemic index, but oddly does not mention grain and legume flours, or high glycemic index fruits, leaving the door open for processed food companies to market products like pasta, cereal and juice beverages to its plant-based planet. High insulin levels strongly increase the risk for numerous chronic diseases and can mean a lifetime of medications, disability, and early death. If the Commission read its own report it would find support for the notion that those of us with metabolic damage may be better off increasing our meat intake and decreasing our carbohydrate intake:
“In a large controlled feeding trial, replacing carbohydrate isocalorically with protein reduced blood pressure and blood lipid concentrations.” [page 8]
This was the 2005 OmniHeart trial, which used 50% plant protein and 50% animal protein. It would seem the only people who should eat a vegan diet are people who make the informed choice to eat a vegan diet, despite the risks.
9. Pay no attention to the money behind the curtain
As an advocate of meat-inclusive diets, I have often been assumed to have financial ties to the meat industry (which I do not), but how many people stop to question the financial (and professional) incentives that may influence doctors promoting plant-based diets? We all have personal beliefs and we all need to make a living, but honesty with oneself and transparency with the public should be paramount. The Nutrition Coalition has compiled a list of Dr. Willett's potential conflicts of interest here.
The EAT Foundation, which collaborated with The Lancet to produce this report, was founded by Norwegian billionaire and animal rights activist Gunhild Stordalen. EAT recently helped to launch "FReSH" (Food Reform for Sustainability and Health), a global partnership of about 40 corporations, including Barilla (pasta), Unilever (meat alternatives and vegetable oils), Kellogg's (cereals) and Pepsico (sugary beverages). Make of this what you will.
10. No to choices, yes to taxes?
How does EAT-Lancet propose to achieve its dream of a plant-based world? Many suggestions are put forth, but two are worth emphasizing: the elimination or restriction of consumer choices, and taxation. The EAT Foundation describes itself as:
"a non-profit startup dedicated to transforming our global food system through sound science, impatient disruption and novel partnerships.”
Sound science? Clearly not. But impatient disruption — what does that mean?
Regardless of how you feel about taxation as a tool for social change, consider the Commission’s own numerous exceptions to the plant-based rules, including pregnant women, children, the malnourished and the impoverished. Should we really support making animal foods — the only nutritionally complete foods on Earth — even more expensive for vulnerable populations? The notion of taxation is followed by a vague reference to the possibility of “cash transfer” social safety nets for women and children. This section of the report is representative of its overall elitist and paternalistic tone.
I believe, because I’m convinced by the science, that animal foods are essential to optimal human health. This is an uncomfortable biological reality we all have to wrestle with as creatures of conscience. Finding ways to support excellent health and quality of life for the creatures we depend on for our sustenance and vitality is one of our most important callings as caring stewards of our planet and all of its inhabitants. But I’m also a firm believer in personal choice. We each need to become experts in what works best for our own bodies. Eat and let eat, I say. It seems clear that EAT-Lancet commissioners are neither supporters of personal choice nor the transparent distribution of accurate nutrition information that would empower people to weigh the risks and benefits of various diets for themselves.
Challenge Authority
The EAT-Lancet report has the feel of a royal decree, operating under the guise of good intentions, seeking to impose its benevolent will on all subjects of planet Earth. It is well worth challenging the presumed authority of this group of 37 “experts,” because it wields tremendous power and influence, has access to billions of dollars, and is likely to affect your health, your choices, and your checkbook in the near future.
Capitalizing on our current public health and environmental crises, the EAT-Lancet Commission pronounces itself as the authority on the science of nutrition, exploits our worst fears, and seeks to dictate our food choices in accordance with its members' personal, professional and possible commercial interests.
To the best of my knowledge, there has never been a human clinical trial designed to test the health effects of simply removing animal foods from the diet, without making any other diet or lifestyle changes such as eliminating refined carbohydrates and other processed foods. Unless and until such research is conducted demonstrating clear benefits to this strategy, the assertion that human beings would be healthier without animal foods remains an untested hypothesis with clear risks to human life and health. Prescribing plant-based diets to the planet without including straightforward warnings of these risks and offering clear guidance as to how to minimize them is scientifically irresponsible and medically unethical, and therefore should not form the basis of public health recommendations.

No comments:
Post a Comment